When the Wires Cross: Living with Autism, ADHD, and Major Neurocognitive Disorder (Post-Radiation Brain Injury)
There are moments when my brain feels like a tangled set of wires — sparks of clarity flickering between darkened circuits. I may lose words, forget paths I once knew, and fumble through conversation, but I’ve learned that resilience isn’t about restoring what was lost. It’s about finding new ways to illuminate what remains.
© thechronicallyresilient
By Frankie — Disabled Air Force Veteran | Chronic Illness Advocate | Social Scientist
Living with autism and ADHD is already complex. The constant juggling act between sensory overwhelm, executive dysfunction, and social decoding takes a tremendous amount of invisible effort. But when you add Major Neurocognitive Disorder (MND) — the medical term for dementia — caused by radiation-induced brain injury after Gamma Knife surgery, the wires of my mind don’t just cross — they sometimes go completely dark.
Understanding the Overlap
Autism and ADHD alone make life a constant negotiation between ability and exhaustion. For me, that meant years of masking — forcing myself to appear “normal,” pushing through sensory chaos, scripting conversations, and maintaining an image of competence even when my brain was on fire inside. But when I developed MND, masking became impossible.
Major Neurocognitive Disorder is often associated with aging, but it can happen at any age. It’s essentially dementia, caused by damage to the brain. In my case, it was a delayed consequence of Gamma Knife radiation used to treat a cerebral arteriovenous malformation — a rare tangle of blood vessels in my brain. What saved my life also fundamentally changed it.
Losing the Words — and Pieces of Myself
There are large chunks of my memory that are simply gone. I can’t recall moments that once shaped who I was. I struggle to find words mid-sentence, my thoughts evaporating before I can anchor them. Sometimes I lose track of what I’m saying entirely.
Conversations that used to feel natural now require enormous concentration. I can’t always interpret tone or filter background noise, and complex instructions leave me frozen. I get confused easily, lost in places I used to navigate without thinking. And every time it happens, I feel a pang of grief — not just for what I’ve lost, but for the people who’ve lost the version of me who could once keep everything straight.
“I used to be dependable — now I’m not, but not at any fault of my own.”
Relationships strain under the weight of my limitations. People assume I’m the same because I still sound articulate, but the truth is, I’m holding things together with fragile threads. My brain works differently now, and no amount of willpower can restore what radiation quietly took from me.
When Masking Becomes Impossible
Before MND, I could still mask my autism and ADHD well enough to survive most social situations. I could prepare scripts, hide overstimulation, and push through burnout. Now, I don’t have that luxury.
The fatigue that comes from cognitive impairment strips away every buffer I once relied on. The filters are gone. My patience for superficiality has worn thin. I say what I mean, even when it’s not what others want to hear. Some call that “difficult.” I call it unfiltered honesty.
“Neurodivergence stripped away my camouflage — but maybe it also stripped me down to my truest self.”
The Loneliness of Not Being Believed
Even doctors sometimes don’t believe me. I’ve become too good at masking my symptoms — at performing competence long enough to pass brief assessments. They see a well-spoken, intelligent adult and assume my brain injury couldn’t be “that bad.” But they don’t see the hours afterward when I crash, disoriented and drained from holding it together.
Being autistic already means living in a world that misunderstands your inner experience. Adding cognitive decline to that creates an isolation that’s hard to describe. It’s a loneliness not just of company, but of comprehension.
The Grief and the Grit
There’s deep grief in realizing that the person I was — the one who could multitask, solve problems, and organize chaos — isn’t coming back. But there’s also resilience in learning how to live differently.
I’ve learned to slow down. To rely on visual aids, notes, alarms, and routines. I give myself grace when I lose words mid-sentence. I find peace in smaller victories — remembering an appointment, finishing a task, making it through a conversation without losing my place.
“This isn’t the life I planned, but it’s still a life worth living — one that demands compassion, creativity, and constant adaptation.”
A Call for Understanding
Major Neurocognitive Disorder doesn’t just happen to the elderly. It can affect people in their 20s, 30s, and 40s — people with families, careers, and lives in progress. It deserves the same level of recognition, research, and empathy as any other neurological condition.
We need more awareness of what it means to live with overlapping neurodivergence and acquired cognitive disability — how it shapes communication, relationships, and identity. I may forget details, lose words, or repeat myself, but I never lose my capacity for love, empathy, meaning and understanding.
So I’ll keep telling my story — even when the sentences come slowly, even when the memories fade. Because somewhere out there, another person is quietly wondering if anyone understands what it’s like when your brain no longer functions the way it once did.
And to them, I want to say: I see you. You’re not broken. You’re rebuilding.
If this story resonates with you, follow my journey @thechronicallyresilient.
And as always, Stay Resilient ❤️🩹
My Brain Tried to Kill Me: Surviving a Cerebral AVM
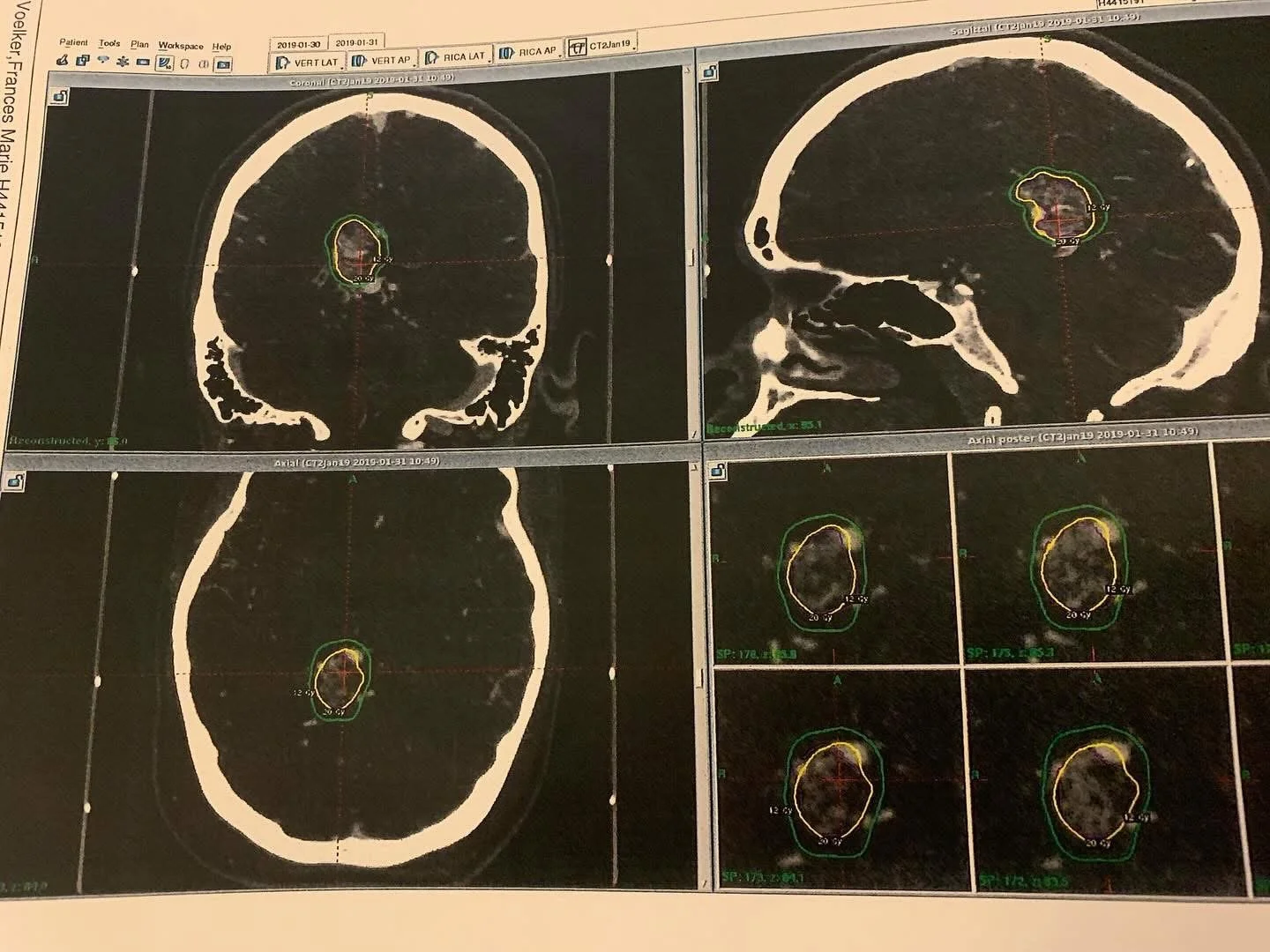
MRI imaging of a cerebral arteriovenous malformation (AVM), showing a complex nidus of abnormal, tangled blood vessels in the brain. This high-grade (Spetzler-Martin Grade 5) AVM carries a significant risk of rupture, necessitating precise intervention and ongoing monitoring.
By Frankie
Disabled Air Force Veteran | Chronic Illness Advocate | Medical Nerd
Hi, I’m Frankie. I’m a 33-year-old disabled Air Force veteran, and I want to tell you about when I learned I had a cerebral arteriovenous malformation (AVM) — and how it almost killed me before I even knew it was there.
This blog is part of my effort to chronicle my medical history in an honest and empowering way — not just for me, but for anyone living with a complex or rare condition. This is my AVM story, and it starts with a whisper in my ear.
What Is a Cerebral AVM?
A cerebral arteriovenous malformation (AVM) is a rare and potentially life-threatening condition where blood vessels in the brain form an abnormal connection between arteries and veins, bypassing capillaries. This creates a tangle of fragile vessels prone to rupture.
Occurs in about 0.05% of the population
Can lead to hemorrhagic stroke if ruptured
Often goes undetected until it bleeds
In my case, I was lucky. My AVM was found before it ruptured — but only because I trusted my instincts and had a provider who listened.
Early Symptoms: When Something Feels Off
In 2018, I started noticing subtle but unusual symptoms:
Pulsatile tinnitus in my right ear (a whooshing sound in rhythm with my heartbeat)
Dizziness and episodes of vertigo
A strange sense that something neurologically wasn’t quite right
These symptoms weren’t severe enough to stop me from functioning, but they persisted — and I couldn’t ignore them.
As a trained Air Force medic, I’d developed a habit of digging deeper into symptoms. I started researching differentials, and one condition kept resurfacing: cerebral AVM. It felt unlikely, but my gut told me not to brush it off.
The MRI That Changed My Life
I confided in a physician I respected deeply — a mentor and colleague. I told him about the symptoms and the concerns I had based on my research.
Instead of dismissing me, he listened.
He ordered an MRI.
I went on a family trip to Hawaii shortly after the scan. When I returned, I hadn’t heard anything, so I checked the results myself at work (as I was authorized to do).
And there it was:
“Cerebral arteriovenous malformation.”
I felt the ground shift beneath me.
A Life-Threatening Diagnosis: Grade 5 AVM
Further evaluation revealed the full picture:
Spetzler-Martin Grade 5 AVM (the highest severity level)
Located in the posterior corpus callosum, deep within the brain
Considered inoperable at the time due to size and location
Here’s the part that really drove it home:
The AVM carried an estimated 3% risk of rupture per year, compounded annually since birth — which translated to a 78% lifetime risk of rupture by the time I was diagnosed.
This wasn’t just serious — it was potentially fatal. But I had options.
My team recommended a non-invasive approach first:
Gamma Knife radiation.
Gamma Knife Radiation: Hope and Risk
In January 2019, I underwent Gamma Knife radiosurgery — a focused radiation treatment designed to gradually shrink the AVM and reduce the risk of rupture.
The procedure itself went well, but soon after, I experienced complications that taught me just how fragile the balance was in my body. Despite the challenges, Gamma Knife was the safest option to treat something inoperable — at least initially.
Why Sharing My Story Matters
Living with a cerebral AVM is a constant reminder of the fragility of life and the power of persistence. Early symptoms can be subtle, and the diagnosis can come as a shock — but timely detection and treatment can save lives.
And if you’re dealing with an AVM, know that you’re not alone. Medical advances and supportive care can make a difference.
Thank you for reading my story. If you found this helpful, please share to raise awareness about cerebral AVMs and the importance of listening to your body.
—
And as always, Stay Resilient ❤️🩹