When the Body Mirrors the Mind: The Connection Between EDS, Autism, and Chronic Survival
For years, I thought my exhaustion was laziness, my pain was weakness, and my dizziness was dehydration. I pushed harder, fought longer, and ignored the quiet signals of my body until I couldn’t anymore. It wasn’t weakness — it was Ehlers-Danlos Syndrome, Autism, and survival. Now I move slower, softer, and more intentionally — not because I’ve given up, but because I’ve finally learned to listen.
© thechronicallyresilient
By Frankie — Disabled Air Force Veteran | Chronic Illness Advocate | Medical Nerd
For most of my life, I lived in survival mode without realizing it. My body was always tight, tense, and unpredictable — pain was constant, fatigue was familiar, and “pushing through” was my default. What I didn’t know back then was that my body wasn’t just tired — it was screaming for understanding.
The Hidden Thread
When I was diagnosed with Autism, ADHD, and Major Neurocognitive Disorder by my neuropsychiatrist who finally saw me as a whole person, something unexpected happened. In the middle of discussing my symptoms, he asked a simple question:
“Are you hypermobile? Do you have stretchy skin?”
No doctor had ever connected those dots with my medical history before. But that question — and the awareness behind it — changed the trajectory of my health. It led to the realization that I also have Hypermobile Ehlers-Danlos Syndrome (hEDS), a connective-tissue disorder that affects collagen throughout the body.
Hypermobile EDS — The Unseen Connection
Unlike other forms of Ehlers-Danlos Syndrome, hEDS doesn’t yet have a definitive genetic marker. It’s complex, often misunderstood, and dismissed for years as “just joint pain” or “being flexible.” But hEDS is more than that — it’s a systemic condition that affects joints, muscles, skin, and even the nervous system.
New research suggests that hEDS may have immunological roots, linking it closely to the neurodivergent population. Many of us who live with Autism and ADHD also show signs of connective-tissue differences — hypermobility, poor proprioception, and heightened sensory awareness. It’s as if our entire nervous system and connective-tissue matrix are speaking the same overstimulated language.
“My connective tissue is as sensitive as my emotions — both overstretch in the wrong environment.”
The Co-Morbidities They Don’t Warn You About
hEDS rarely comes alone. It brings a whole entourage of conditions that impact every system of the body. For me, that includes:
• POTS (Postural Orthostatic Tachycardia Syndrome): a form of dysautonomia that makes my heart race and blood pressure drop when I stand up. Some days, even showering or walking across the room feels like climbing a mountain.
• Gastroparesis: slow digestion that leaves me nauseated, bloated, and struggling to eat foods that once brought comfort.
• MCAS (Mast Cell Activation Syndrome): my body can overreact to harmless triggers — foods, scents, or temperature changes — causing hives, swelling, or even anaphylaxis without warning.
• Chronic Hypotension: low blood pressure that leaves me dizzy, foggy, and drained.
• Chronic Dehydration: because of how connective-tissue and autonomic dysfunction affect fluid balance, people with EDS often struggle to stay hydrated no matter how much water they drink. Electrolytes help, but the dehydration is physiological — not neglectful.
Each condition on its own is challenging; together, they create a body that’s constantly negotiating stability.
“My autonomic system forgot how to be automatic — so now I have to consciously manage what most people’s bodies do effortlessly.”
When “Just Work Out More” Isn’t the Answer
For most of my life, I thought my exercise intolerance was just me being “out of shape.” I was told to push harder, work out more, drink more water. But the thing is — that wasn’t true.
No matter how hard I tried, my body would crash. I’d get dizzy, lightheaded, nauseated, and overwhelmed by pain that lingered for days afterward. I thought everyone lived that way — constantly sore, constantly exhausted, always pushing through headaches, dizziness, and discomfort. But they don’t.
And yes, dehydration was part of the problem — but not in the way people assumed. For those with EDS and POTS, dehydration isn’t from lack of effort; it’s a symptom of our physiology. Our bodies can’t retain fluids properly, and our blood vessels don’t constrict as they should. No amount of water could fix that.
“I spent decades apologizing for symptoms that were never my fault — I just didn’t have the right language to name them.”
Living in Constant Survival Mode
Chronic pain trains the nervous system to stay on high alert, and autism compounds that hypervigilance. The sensory system doesn’t just process the world differently — it feels it differently. Every sound, texture, or light can amplify pain and fatigue.
That’s why so many autistic and EDS individuals live in a permanent state of fight, flight, or freeze. Our bodies aren’t malfunctioning; they’re overprotecting. When the connective tissue can’t support the body properly, the brain compensates by tightening muscles, increasing stress hormones, and scanning constantly for danger.
It’s survival — not choice.
Managing the Unmanageable
Living with EDS and its co-morbidities means every day is a careful balancing act between pushing and protecting. Healing isn’t passive — it’s an ongoing conversation with my body.
I do aquatic physical therapy two to three times a week when I can, because the water supports my joints while letting me move freely. It’s low-impact but strengthens my muscles and helps my cardiovascular system without triggering a flare. When I’m not in the pool, I aim for light cardio walks of one to three miles and try to lift weights several times per week to maintain muscle tone and joint stability.
These aren’t vanity routines — they’re survival ones. If I stop moving, my joints destabilize. If I overdo it, I crash. So every workout becomes a dialogue: What can my body handle today?
Because of low hunger drive, absent appetite, and chronic nausea, I use an app to track calories to prevent unintentional weight loss. Eating isn’t just about food — it’s structured self-care that keeps me functional.
And I go to therapy every other week, because when you live inside a body that constantly demands negotiation, you need a place to process the emotional weight too. Talking helps me release the guilt, fear, and exhaustion that come with chronic illness.
“Therapy keeps my mind flexible when my body can’t be. Movement keeps my body alive when my mind feels heavy.”
None of this is easy. Some weeks I’m strong; others I’m surviving hour by hour. But each step — in the water, on the trail, or in the therapist’s office — is a reminder that I’m still here, still adapting, still moving forward with purpose.
The Diagnosis That Finally Made Sense
When my neuropsychiatrist mentioned hypermobility, something clicked. I thought about all the sprains, the fatigue, the bruises that appeared out of nowhere, and the deep aches I’d brushed off as “normal.” I thought about how often I felt like my body and brain were out of sync — my mind racing while my body lagged behind, or vice versa.
That single moment of recognition reframed my entire past. It explained the chronic pain, the joint instability, the exhaustion after simple tasks. It even explained why sensory overload felt like physical injury — because in a way, it was. My body and mind were both running emergency protocols, just trying to survive.
“For the first time, I wasn’t broken — I was understood.”
Looking Back with Compassion
I look back now and see how much of my life was shaped by this unseen battle between my connective tissue and my nervous system. The anxiety that doctors misread as psychological was actually physiological. The fatigue that looked like laziness was the cost of existing in a body that never felt safe.
I used to think I was weak for not being able to keep up — now I know I was fighting on multiple fronts. My body was working overtime to hold me together, even as my mind tried to make sense of it all.
Living with the Body and Mind That I Have
Living with hEDS, Autism, ADHD, and Major Neurocognitive Disorder means existing at the crossroads of neurology, genetics, and survival. But it also means I’ve learned to read the language of my body — every ache, every tremor, every flare. They’re messages, not malfunctions.
And now that I finally understand them, I can live with more compassion, more grace, and more intention than ever before.
If this story resonates with you I hope you’ll stick around, follow my journey @thechronicallyresilient.
And as always, Stay Resilient ❤️🩹
When the Wires Cross: Living with Autism, ADHD, and Major Neurocognitive Disorder (Post-Radiation Brain Injury)
There are moments when my brain feels like a tangled set of wires — sparks of clarity flickering between darkened circuits. I may lose words, forget paths I once knew, and fumble through conversation, but I’ve learned that resilience isn’t about restoring what was lost. It’s about finding new ways to illuminate what remains.
© thechronicallyresilient
By Frankie — Disabled Air Force Veteran | Chronic Illness Advocate | Social Scientist
Living with autism and ADHD is already complex. The constant juggling act between sensory overwhelm, executive dysfunction, and social decoding takes a tremendous amount of invisible effort. But when you add Major Neurocognitive Disorder (MND) — the medical term for dementia — caused by radiation-induced brain injury after Gamma Knife surgery, the wires of my mind don’t just cross — they sometimes go completely dark.
Understanding the Overlap
Autism and ADHD alone make life a constant negotiation between ability and exhaustion. For me, that meant years of masking — forcing myself to appear “normal,” pushing through sensory chaos, scripting conversations, and maintaining an image of competence even when my brain was on fire inside. But when I developed MND, masking became impossible.
Major Neurocognitive Disorder is often associated with aging, but it can happen at any age. It’s essentially dementia, caused by damage to the brain. In my case, it was a delayed consequence of Gamma Knife radiation used to treat a cerebral arteriovenous malformation — a rare tangle of blood vessels in my brain. What saved my life also fundamentally changed it.
Losing the Words — and Pieces of Myself
There are large chunks of my memory that are simply gone. I can’t recall moments that once shaped who I was. I struggle to find words mid-sentence, my thoughts evaporating before I can anchor them. Sometimes I lose track of what I’m saying entirely.
Conversations that used to feel natural now require enormous concentration. I can’t always interpret tone or filter background noise, and complex instructions leave me frozen. I get confused easily, lost in places I used to navigate without thinking. And every time it happens, I feel a pang of grief — not just for what I’ve lost, but for the people who’ve lost the version of me who could once keep everything straight.
“I used to be dependable — now I’m not, but not at any fault of my own.”
Relationships strain under the weight of my limitations. People assume I’m the same because I still sound articulate, but the truth is, I’m holding things together with fragile threads. My brain works differently now, and no amount of willpower can restore what radiation quietly took from me.
When Masking Becomes Impossible
Before MND, I could still mask my autism and ADHD well enough to survive most social situations. I could prepare scripts, hide overstimulation, and push through burnout. Now, I don’t have that luxury.
The fatigue that comes from cognitive impairment strips away every buffer I once relied on. The filters are gone. My patience for superficiality has worn thin. I say what I mean, even when it’s not what others want to hear. Some call that “difficult.” I call it unfiltered honesty.
“Neurodivergence stripped away my camouflage — but maybe it also stripped me down to my truest self.”
The Loneliness of Not Being Believed
Even doctors sometimes don’t believe me. I’ve become too good at masking my symptoms — at performing competence long enough to pass brief assessments. They see a well-spoken, intelligent adult and assume my brain injury couldn’t be “that bad.” But they don’t see the hours afterward when I crash, disoriented and drained from holding it together.
Being autistic already means living in a world that misunderstands your inner experience. Adding cognitive decline to that creates an isolation that’s hard to describe. It’s a loneliness not just of company, but of comprehension.
The Grief and the Grit
There’s deep grief in realizing that the person I was — the one who could multitask, solve problems, and organize chaos — isn’t coming back. But there’s also resilience in learning how to live differently.
I’ve learned to slow down. To rely on visual aids, notes, alarms, and routines. I give myself grace when I lose words mid-sentence. I find peace in smaller victories — remembering an appointment, finishing a task, making it through a conversation without losing my place.
“This isn’t the life I planned, but it’s still a life worth living — one that demands compassion, creativity, and constant adaptation.”
A Call for Understanding
Major Neurocognitive Disorder doesn’t just happen to the elderly. It can affect people in their 20s, 30s, and 40s — people with families, careers, and lives in progress. It deserves the same level of recognition, research, and empathy as any other neurological condition.
We need more awareness of what it means to live with overlapping neurodivergence and acquired cognitive disability — how it shapes communication, relationships, and identity. I may forget details, lose words, or repeat myself, but I never lose my capacity for love, empathy, meaning and understanding.
So I’ll keep telling my story — even when the sentences come slowly, even when the memories fade. Because somewhere out there, another person is quietly wondering if anyone understands what it’s like when your brain no longer functions the way it once did.
And to them, I want to say: I see you. You’re not broken. You’re rebuilding.
If this story resonates with you, follow my journey @thechronicallyresilient.
And as always, Stay Resilient ❤️🩹
The Bullet That Didn’t Kill Him — But Almost Killed Me: A Story of Childhood Trauma, Silence, and Survival
Seventeen years after the accident, I finally harvested my first mule deer doe. Not for sport — but for healing. For the girl who thought she’d never pick up a rifle again, and the woman who learned she could.
By Frankie — Disabled Air Force Veteran | Chronic Illness Advocate | Medical Nerd
⚠️ Trigger Warning: This story discusses a firearm accident, childhood trauma, and references to suicidal thoughts. Reader discretion advised.
Some moments don’t just change you — they grow you up before you know how to be grown.
I was 12 years old the day I stopped being a child.
And it happened in the wide-open sagebrush country of eastern Montana — a place I once loved for its freedom and silence.
A place that would go silent in a whole new way that day.
The First Harvest and the Shot That Shouldn’t Have Happened
“I was walking up on my first buck, full of pride and innocence — within seconds, everything I knew about safety, confidence, and who I thought I was shattered.”
It was my first year hunting, just two years after completing hunter’s safety — which in Montana isn’t just a class; it’s a rite of passage.
I was with my father, grandfather, and brother. We’d split up at first, planning to meet back at a predetermined ridge. I was over the moon — I’d just shot my first mule deer buck. A 4x5. He was beautiful. I was proud. I had arrived.
As I walked up to the animal, I turned to look back — thinking no one was behind me.
I was wrong.
In a split-second that still plays in slow motion in my mind — my rifle suddenly fired.
There was no warning. No conscious pull of the trigger. The sound shattered the sky and hollowed my hearing. My vision darkened. I felt frozen inside a body that had just experienced something I couldn’t comprehend.
When my hearing and sight started to return, they came back in pieces — first the ringing, then the panic, and then my dad’s voice:
“FRANKIE!! FRANK!! START RUNNING! CHASE THAT TRUCK! RUN!!”
His voice wasn't calm. It was pure panic, urgency, and fear.
And it snapped me into action.
A Run for Help — And a Moment I’ll Never Forget
I took off running.
The sage tore at my legs. My lungs seared. I stumbled, fell, got back up. I screamed so hard nothing came out. I just ran until I caught up to a truck, waving my arms, begging it to stop.
The truck finally did.
A tall man with dark hair in a red plaid jacket and hunter’s orange vest jumped out of the cab and ran toward me. I collapsed into his arms, shaking, barely able to breathe.
I somehow managed to say:
“My grandpa — he’s been shot! It was an accident.”
He grabbed his radio instantly and called it in. We were instructed to meet the ambulance on the highway.
My brother and I turned to wait for our dad and grandfather.
And then — I saw them.
The Only Voice That Spoke Truth
My grandfather didn’t collapse where he stood.
He walked half a mile — with a bullet in his abdomen — up to the road where I was waiting by my dad’s Bronco. He was holding his side, pale, sweating, covered in pain and determination.
When he reached me, he didn’t speak at first.
He just handed me his binoculars — the ones the bullet had ricocheted off of, the ones that had saved his life.
Then he laid down on the ground with his head in my lap.
He looked up at me with eyes half-lidded from pain and said:
“I'm tired, Frankie. Don’t let me go to sleep.”
I’ll never forget the weight of him in my lap — or the terror of believing I might lose him right then and there, in my arms, not during a hunt, but because of something I couldn’t even make sense of.
After that, he climbed into my dad’s Bronco, and we drove to meet the waiting ambulance.
He survived.
“I remember the world going silent — and the silence stayed long after the sound of the shot was gone.”
The Silence That Followed
After surgery, I was the first person he wanted to see.
He held my hand and told me:
“This was not your fault. I don’t blame you. I’m not mad.”
I believed him — or tried to.
But no one else said those words.
My grandmother wouldn’t look at me. The adults went quiet. The police questioned me.
And after one brief session with a school therapist, I was deemed “fine.”
I wasn’t fine.
When Trauma Is Treated Like a Fluke
Childhood trauma isn’t just about what happens to you.
It’s about what happens after.
When adults don’t talk to you, don’t help you process, don’t believe you — the wound goes uncleaned.
Unfelt pain doesn’t vanish.
It festers.
It waits.
Growing Up in the Quiet
For years, I replayed that day over and over, trying to make sense of it.
Trying to figure out how the rifle fired.
Trying to understand what I’d done — and why no one was talking about it.
I knew my finger wasn’t on the trigger. I knew I followed the rules. I knew I hadn’t reloaded — and yet I was the one the police pulled aside. I was the one who got quiet stares. I was the one who went silent — because silence seemed safer than saying, “I don’t understand what happened.”
But staying silent came at a cost.
I didn’t just stop being a child that day — I stopped knowing how to be alive in a world that expected me to carry on as if nothing had happened.
I internalized the blame.
I turned the confusion and guilt inward.
I became afraid of myself — afraid of what I’d done, and what I might do.
I was terrified, constantly, that I was capable of causing harm without knowing how or why.
And no one saw it.
No one checked in after the hospital.
No one asked how I was sleeping, or if I was eating.
I withdrew.
I masked.
And as a result — I spiraled.
Nights were the worst. I had vivid nightmares. Terrifying reenactments. Sweaty flashbacks I couldn’t escape from.
And slowly, without language for what I was feeling, the only escape I saw was not being alive anymore.
I was a child silently contemplating death — because I thought that was the only way to escape what I'd allegedly done.
That’s what untreated trauma does — especially to an undiagnosed autistic kid with ADHD living in an abusive home, where feelings weren’t safe and silence was survival.
When you learn that your pain isn’t welcome, you stop showing it.
And when you're never taught how to process the unbearable, it turns inward.
A Question That Changed Everything
Years later, when I was finally diagnosed with PTSD, my psychiatrist asked me something I had never allowed myself to consider:
“Frankie, your father is an alcoholic and you know your finger wasn’t on the trigger. What if your father was the one who accidentally shot your grandfather… and you were made to believe it was you?”
That question changed everything.
It cracked open years of silence and self-blame, forcing me to see the possibility that the story I’d carried might never have been entirely mine to bear. I may never know the full truth — but I know that little girl deserved to be believed, protected, and guided through this.
Instead, she was left to survive the weight of everyone else’s fear.
How I Reclaimed the Wild
I didn’t go back to hunting for fourteen years.
It wasn’t until I met my husband in 2018 that I picked up a rifle again and it would be three more years before I harvested my first deer seen in the picture above
.
With him, hunting became something different — not about ego or perfection, but about connection, sustainability, and healing.
It was the first time I saw hunting as a way to reclaim the parts of myself I’d buried.
To step back into the wild without fear — and with reverence.
Now, even with POTS, brain injury, significant hearing loss and auditory and visueal processing issues, visual impairment, and neuro fatigue — I still go.
Not to prove I’m capable.
But to remind myself that I still belong.
Because the wild didn’t abandon me — people did.
For the Child I Was and the Woman I Am
If I could speak to that 12-year-old girl now, I’d tell her:
You didn’t do anything wrong.
There were layers of things working against you.
You followed the rules.
And the silence that followed wasn’t your fault either.
You didn’t deserve the blame.
You didn’t deserve the shame.
You didn’t deserve to be alone in that pain.
And one day — you’ll find your way back to those sage-covered hills.
Not as the child who fell —
But as the woman who rose.
If this story speaks to anything you’ve carried alone — childhood trauma, chronic illness, neurodivergence, or the long road back to yourself — I hope you’ll stay with me, follow along @thechronicallyresilient.
And as always, Stay Resilient. ❤️🩹
Navigating a Complex Diagnosis: My Journey Through Rare Disease, Chronic Illness, and Advocacy
After years of surviving rare conditions, medical errors, and the fallout of life-saving treatment, I’ve learned one truth: sometimes you have to become your own advocate just to stay alive. As a disabled Air Force veteran living with complex chronic illnesses, I use every tool available — including AI — to organize the chaos, tell my story, and fight for better care. This post shares how a missed diagnosis of hyperparathyroidism exposed deeper flaws in the VA system and why trusting your instincts can truly save your life.
By Frankie
Disabled Air Force Veteran | Chronic Illness Advocate | Medical Nerd
Hi, I’m Frankie — I’m 33 years old, a disabled Air Force veteran, and someone living with multiple complex medical conditions. I’m sharing my story not for sympathy, but in hopes of helping others feel seen, advocating for change, and holding space for anyone navigating a healthcare system that doesn’t always listen the first time — or even the tenth.
This blog is my way of organizing the chaos. I use tools like AI and technology to help structure my thoughts, because as someone with autism, ADHD, and a major neurocognitive disorder, communicating clearly and logically has become a real challenge. Masking is something I do well — on the outside, I may look "put together," but beneath that is a network of alarms, calendars, checklists, detailed notes, and the support of my husband.
Today, I want to talk about one of my most urgent health issues — undiagnosed and untreated hyperparathyroidism— and how it slipped through the cracks of the VA system for over two years.
In 2023, the VA flagged elevated calcium levels in my labs and entered a referral for Endocrinology. I had no idea. No call. No message. No follow-up. Nothing. I didn't find out until nearly a year later, when Care in the Community called me to ask if I was ready to move forward with my endocrinology appointment — a referral I never knew existed.
This should have never happened.
In August 2024, I finally had my parathyroid hormone (PTH) level checked — and it was elevated at 87, a result that should have immediately prompted further investigation. I was referred again to Endocrinology, but they declined to see me because my calcium levels looked “normal.”
Here’s what they missed: elevated PTH with normal calcium can indicate Normocalcemic Primary Hyperparathyroidism (NPHPT). It’s real, it’s documented, and it’s serious. But it requires a provider who understands the nuance — and who’s willing to dig deeper.
I’ve become symptomatic. Yes, I have fatigue from Ehlers-Danlos Syndrome, but this is different. Since August, my energy levels have dropped sharply. My sleep is unpredictable and fragmented. I now wake between 2–4 AM every day, even when I’m completely exhausted. My go-to sleep supports — including THC — have stopped working.
I'm scared that this will lead to another major flare. I’ve worked too hard to stabilize. I can’t afford to lose access to treatments, especially medications like those for ADHD, which my psychiatrist won’t prescribe if I start losing weight again.
From Air Force Medic to Full-Time Patient
Before I became a full-time patient, I was a medic in the Air Force. For seven years, I thrived in high-pressure medical environments, trained and mentored junior medics, and earned the respect of my colleagues. Medicine wasn’t just a job — it became my language, my special interest, and my safe place as an autistic person.
That experience shaped me into the kind of patient I am today — proactive, hyper-organized, and relentless when it comes to advocating for myself. Not because I think I know more than my doctors, but because I’ve learned the hard way that if I don’t stay on top of every detail, I’ll fall through the cracks.
And I already have.
The Day My Instinct Saved My Life
In early 2019, I underwent Gamma Knife radiation surgery to shrink a massive cerebral arteriovenous malformation (AVM) that carried a 78% lifetime risk of rupture. About a week later, I noticed swelling and pain in my right arm where I’d had an IV. The NP said it was probably just phlebitis. My heart rate was elevated, but they weren't concerned.
Still, something didn’t feel right.
I went to the ER. They found a thrombosis in my basilic vein and a highly elevated D-dimer. A chest CT revealed something terrifying: bilateral pulmonary emboli in all four lobes of my lungs. I was completely asymptomatic. No chest pain. No shortness of breath. Just a gut feeling and a racing heart.
If I had gone home instead of trusting my instinct, I might not be here writing this.
AVM Diagnosis: Another Case of “It’s Probably Nothing”
Backtracking a few months — in late 2018, I began experiencing pulsatile tinnitus, dizziness, and vertigo. It could have been anything. Still, I mentioned to a trusted physician mentor that I’d done some research and wondered about an AVM. He agreed it was worth looking into. He ordered the MRI.
That scan revealed a Spetzler-Martin Grade 5 AVM in my posterior corpus callosum — one of the rarest and most dangerous types. Most people don’t know they have an AVM until it ruptures. Mine didn’t. That MRI may have saved my life.
The Aftermath: Radiation, Hearing Loss, and Cognitive Decline
Within six months of radiation, I lost hearing in my left ear. Within a year, I lost hearing in my right. By two years post-op, I could no longer work due to memory loss, difficulty with cognition, and executive dysfunction.
Eventually, I was diagnosed with Major Neurocognitive Disorder, Autism, ADHD, and a math disability. I'm now under active neurological evaluation to determine whether the Gamma Knife radiation — which research confirms can cause both cognitive decline and hearing loss — is the root cause.
For years, I begged doctors to help me understand what was happening to my brain. They told me it wasn’t serious. That I was overreacting. That it was stress.
It wasn’t.
Layers of Complexity: A Web of Diagnoses
The deeper you go into my medical history, the more tangled it becomes — but each piece matters. Here’s a brief look at the major players:
Cerebral AVM (diagnosed 2018, resected 2024)
Pulmonary Sarcoidosis (diagnosed 2020, in remission with annual PFT follow-ups)
Hypermobile Ehlers-Danlos Syndrome (diagnosed 2022)
POTS, Dysautonomia, Orthostatic Hypotension
Gastroparesis, Chronic Nausea
Mast Cell Activation Syndrome
Epilepsy Partialis Continua (controlled on Keppra)
Major Neurocognitive Disorder
Autism, ADHD (Inattentive Type), PTSD
Bilateral Sensorineural Hearing Loss
Military Sexual Trauma Survivor
I use a central port to self-administer fluids twice per week to stay hydrated and prevent fainting. My medications and therapies are tightly coordinated and managed across multiple specialists.
But even with all of this, my recent experience with hyperparathyroidism shows how easy it is for critical care to be missed.
Where I Am Now — And What I Need
Right now, I need a thorough evaluation of my parathyroid function. I want answers, not assumptions. I want an Endocrinologist who understands that normal calcium doesn’t rule out parathyroid disease. I need someone who will look at my full history, not just a snapshot.
This isn’t just about one lab result. It’s about an entire system that repeatedly fails to see the bigger picture — and patients like me, who don’t fit into neat diagnostic boxes.
Thankfully, I’m still fighting. I have providers who listen. I have a neurologist who’s taking my cognitive issues seriously. I’m hopeful. But I also know that without constant advocacy — from me, from my support system, and from people like you — none of this moves forward.
For Anyone Reading This
Whether you're a fellow chronically ill person, a caregiver, a provider, or just someone trying to understand — thank you for reading. If you take away one thing from this, let it be this:
🟣 Listen to your body.
🟣 Advocate even when you're tired.
🟣 Trust your instincts — they might just save your life.
Stay tuned for a weekly Blog, Mondays at 1500 (3PM MST)
Stay resilient,
Frankie
My Brain Tried to Kill Me: Surviving a Cerebral AVM
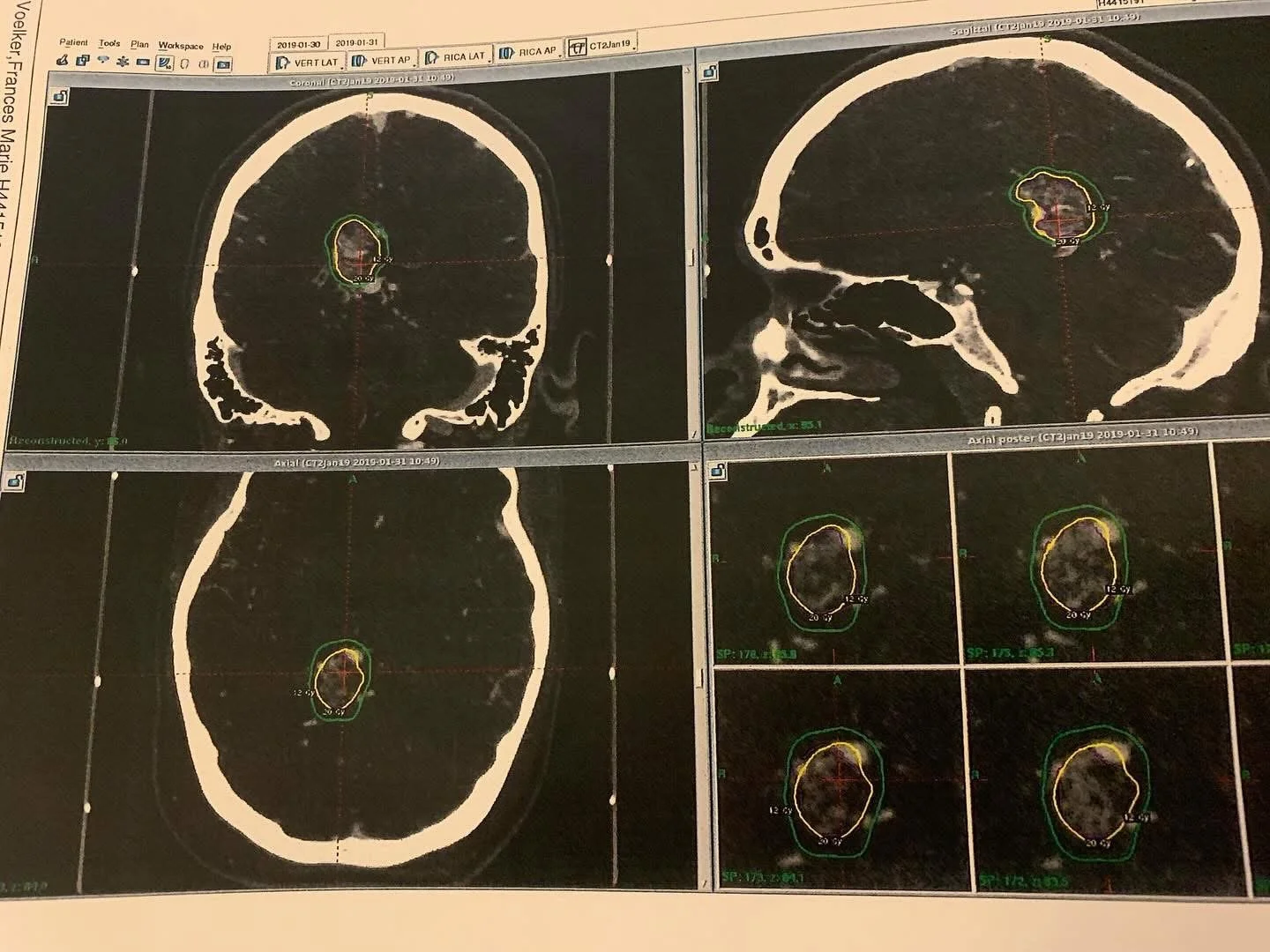
MRI imaging of a cerebral arteriovenous malformation (AVM), showing a complex nidus of abnormal, tangled blood vessels in the brain. This high-grade (Spetzler-Martin Grade 5) AVM carries a significant risk of rupture, necessitating precise intervention and ongoing monitoring.
By Frankie
Disabled Air Force Veteran | Chronic Illness Advocate | Medical Nerd
Hi, I’m Frankie. I’m a 33-year-old disabled Air Force veteran, and I want to tell you about when I learned I had a cerebral arteriovenous malformation (AVM) — and how it almost killed me before I even knew it was there.
This blog is part of my effort to chronicle my medical history in an honest and empowering way — not just for me, but for anyone living with a complex or rare condition. This is my AVM story, and it starts with a whisper in my ear.
What Is a Cerebral AVM?
A cerebral arteriovenous malformation (AVM) is a rare and potentially life-threatening condition where blood vessels in the brain form an abnormal connection between arteries and veins, bypassing capillaries. This creates a tangle of fragile vessels prone to rupture.
Occurs in about 0.05% of the population
Can lead to hemorrhagic stroke if ruptured
Often goes undetected until it bleeds
In my case, I was lucky. My AVM was found before it ruptured — but only because I trusted my instincts and had a provider who listened.
Early Symptoms: When Something Feels Off
In 2018, I started noticing subtle but unusual symptoms:
Pulsatile tinnitus in my right ear (a whooshing sound in rhythm with my heartbeat)
Dizziness and episodes of vertigo
A strange sense that something neurologically wasn’t quite right
These symptoms weren’t severe enough to stop me from functioning, but they persisted — and I couldn’t ignore them.
As a trained Air Force medic, I’d developed a habit of digging deeper into symptoms. I started researching differentials, and one condition kept resurfacing: cerebral AVM. It felt unlikely, but my gut told me not to brush it off.
The MRI That Changed My Life
I confided in a physician I respected deeply — a mentor and colleague. I told him about the symptoms and the concerns I had based on my research.
Instead of dismissing me, he listened.
He ordered an MRI.
I went on a family trip to Hawaii shortly after the scan. When I returned, I hadn’t heard anything, so I checked the results myself at work (as I was authorized to do).
And there it was:
“Cerebral arteriovenous malformation.”
I felt the ground shift beneath me.
A Life-Threatening Diagnosis: Grade 5 AVM
Further evaluation revealed the full picture:
Spetzler-Martin Grade 5 AVM (the highest severity level)
Located in the posterior corpus callosum, deep within the brain
Considered inoperable at the time due to size and location
Here’s the part that really drove it home:
The AVM carried an estimated 3% risk of rupture per year, compounded annually since birth — which translated to a 78% lifetime risk of rupture by the time I was diagnosed.
This wasn’t just serious — it was potentially fatal. But I had options.
My team recommended a non-invasive approach first:
Gamma Knife radiation.
Gamma Knife Radiation: Hope and Risk
In January 2019, I underwent Gamma Knife radiosurgery — a focused radiation treatment designed to gradually shrink the AVM and reduce the risk of rupture.
The procedure itself went well, but soon after, I experienced complications that taught me just how fragile the balance was in my body. Despite the challenges, Gamma Knife was the safest option to treat something inoperable — at least initially.
Why Sharing My Story Matters
Living with a cerebral AVM is a constant reminder of the fragility of life and the power of persistence. Early symptoms can be subtle, and the diagnosis can come as a shock — but timely detection and treatment can save lives.
And if you’re dealing with an AVM, know that you’re not alone. Medical advances and supportive care can make a difference.
Thank you for reading my story. If you found this helpful, please share to raise awareness about cerebral AVMs and the importance of listening to your body.
—
And as always, Stay Resilient ❤️🩹